Drs. Kwang-Bum Park, Myung-Hwan An, Sang-Taek Lee, Young-Jin Lee, Hyun-Jin Kim, Woo-Chang Noh, and Hyun-Wook An present their findings on the survival rates of the XPEED® implant system
Since the concept of osseointegration was introduced by Brånemark in the 1960s, implants have been widely recommended in the arena of dental treatment with high success rates being reported (Brånemark, et al., 1969; Rosenberg, et al., 2004; Hämmerle, et al., 2002; Bahat, 2000).
Many authors claim one prerequisite for successful osseointegration is initial stability (Martinez, et al., 2001) after implant placement, which depends on the surface characteristics and morphology of the implant and the bone density of the surgical site (Meredith, 1998; Barewal, 2003). At any given time, a number of surface treatment methods are being researched to facilitate rapid, strong osseointegration.
Many studies have been performed on implant success rates, and a number of different factors are known to be involved in the long-term success of implants.The height of the marginal bone in particular has been found to be a very important factor in determining the functional and esthetic success of implants, meaning maintaining appropriate height of marginal bone is a prerequisite for a satisfactory long-term result. 
After Schnitman, et al. (1979), presented their criteria for implant success, and many other criteria followed (Smith and Zarb, 1989; Misch, 1998; Buser, et al., 1999), but the most widely used in modern practice are arguably the criteria proposed by Albrektsson, et al., in 1986.
These criteria detail no implant mobility, no translucency on radiographs, no symptoms such as pain or numbness, and bone resorption of 1.5 mm or less in the first year following prosthetic connection, 0.2 mm or less per year following that, and a minimum 85% success rate at 5 years and 80% at 10 years.
Recently, various types of implants have been introduced to the market, and the advancement of implant systems and procedures have helped the success rate rise to as much as 95% or higher as suggested by many papers in the last decade.
This article will discuss the outcome of a study conducted into the success rates of the ExFeel® External implant system, an external connection-type implant using the XPEED® surface and sold by MegaGen.
Using hydroxyapatite, the XPEED surface is treated with resorbable blast media (RBM) that increases the affinity to bone, followed by infiltration of Ca2+ into the surface to form a calcium titanate nano-structure. Of late, many in vivo and in vitro studies have been performed on titanium with Ca2+ ion on the surface.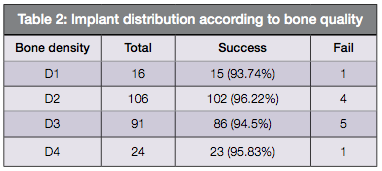
Park, et al. (2009), reported that the nano-structure formed by Ca2+ treatment enhances osteoconductivity. Lee, et al. (2011), reported that the XPEED surface treatment improves apatite formation, loosening torque, and bone to implant contact (BIC). The XPEED surface treatment is continually advancing, but the reality is that a new implant surface meets resistance due to lack of verification on its long-term safety.
The objective of this study was therefore to retrospectively examine the survival rate, and at the same time verify the usefulness, of the ExFeel External implant system by analyzing the patients treated with the implant system in terms of distribution of gender, age, implant location, additional surgery, and final prosthetic type.
Materials and methods:
Study subjects
The study includes 111 patients who had implant surgery performed at Daegu MIR Dental Hospital, Suncheon MIR Dental Hospital, or Kimhyunjin Dental Clinic in Korea from August 2010 and were followed up for 2 to 3 years until March 2013. The average age of the patients was 55.2 years old, of which 67 were men and 44 were women. A total of 237 implants were placed: 127 of them in men and 110 in women, with 74 in the maxilla and 163 in the mandible.
Study materials
The study looked at the externally-connected straight-type ExFeel system with XPEED surface. The implant is available in diameters of 3.3 mm, 3.75 mm, 4 mm, 4.5 mm, 5 mm, and 5.5 mm and in lengths of 7 mm, 8 mm, 10 mm, 11 mm, and 13 mm. In this study, 4 mm or 5 mm diameter implants with a length of 10 mm were placed.
Study method
Using medical charts of patients, the following was looked into:
- Gender of patients, implant distribution, and locations
- Bone quality of implant site and primary stability
- Placement timing and the use of guided bone regeneration
- Implant survival rate
An oral examination and radiograph test were also carried out on all the patients, and their smoking status was also checked.
 Results
Results
Demographics and implant distribution – A total of 237 ExFEEL external fixtures were placed on 111 patients. Out of these, 127 implants (53.6%) were placed in 67 men (60.4%) and 110 (46.4%) in 44 women (39.6%).
In men, seven out of the 127 implants placed failed and 120 (94.48%) succeeded. In women, four out of 110 implants placed failed, and 106 (96.36%) survived — women showed some 1.9% higher survival rate than men (Figure 1A).
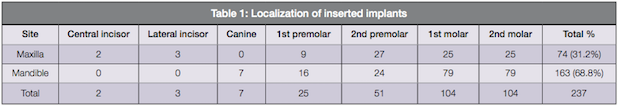
Out of 237 implants in total, 74 (31.2%) were placed in the maxilla and 163 (66.8%) in the mandible as twice more implants were placed in the mandible than the maxilla concentrating on left and right molar regions (Table 1).
In the maxilla, six out of 74 inserted implants failed, and 68 (91.89%) survived; and in the mandible, five out of 163 inserted implants failed, and 158 (96.93%) survived, with about 5% better survival rate in the mandible than the maxilla (Figure 1B).
Bone quality and primary stability – The bone quality of implant patients was categorized according to Lekholm classification. In the order of frequency, type II (106), type III (91), type IV (24), and type 1 (16) were observed (Table 2).
Placement timing and guided bone regeneration – In terms of implant placement timing, 189 implants were placed in healed ridges, 28 were immediately placed, and 20 placed with a delayed approach in the order of frequency. In 28 cases of immediate placement, five cases failed. All 20 delayed cases (100%) survived, and of the 189 cases placed in healed ridges, six failed (Table 3).
In 74 guided bone regeneration (GBR) cases, five failed. Of the 34 socket regeneration cases, three failed, and all 28 sinus lift cases survived. Of the 101 cases carried out without GBR, three failed (Table 4).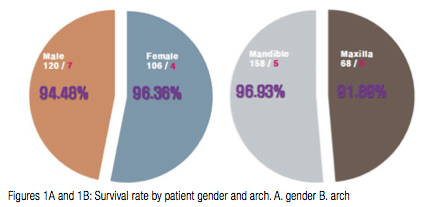
Survival analysis
A total of 237 implants were placed, and 226 of them were still surviving at 3 months following the placement. Of these surviving implants, all 226 of them went on to survive for more than 2 years (Table 5).
Analysis of failed implants
There were 11 implants that did not meet the survival criteria, including one osseo-integration failure with occlusal problems, three due to smoking and drinking, one burned because of bone quality, two lost by infection, and four loosened after immediate placement or failure to integrate (Table 6).
Discussion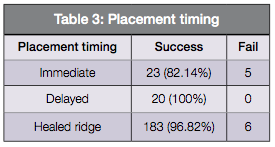
A number of in vivo and in vitro studies have recently been conducted on titanium with Ca2+ ion surfaces. The subject of this particular study was the ExFeel External implant system manufactured by the Korean company, MegaGen.
It has an external abutment connection, and features self-tapping threads and cutting edges for good primary stability. Using hydroxyapatite, the surface is treated with resorbable blast media (RBM) with the aim of promoting affinity to bone followed by infiltration of the Ca2+ ion into the surface to form a calcium titanate nano-structure (Park, et al., 2009).
The survival rate of implants was defined as the ratio of implants remaining in the mouth and not removed due to failure at the time of the study.
The criteria for implant failure was taken to include mobile implant fixtures, translucency on radiograph around the implant during healing, a failure to osseointegrate as determined by the fixture rotating when the healing abutment was connected, uncontrolled pain, infection, and neurological abnormalities (Cochran, et al., 2002; Seong-Leon and Young-Kyun, 2010).
The most widely used implant success criteria by Albrektsson, et al. (1986), also treats the year following implant placement as a critical timescale. The loading of the implant is reflected in the 1-year data; most prostheses would be completed within a year of placement (Carr, et al., 2003). 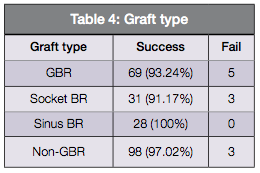
Survival table analysis was used in this study based on the assessment of cumulative survival rate (CSR). To assess the cumulative survival rate with 95% confidence level, the data is usually analysed for a duration of 5 years with assessment performed every year. This method is used in many studies to assess CSR of implants (Cutler and Ederer 1958; Chuang, et al., 2001).
In many studies assessing implants, a modified survival table is applied depending on follow-up period, implant placement, or prosthesis criteria. For this study, it was modified in units of 5 months to assess the 1-year CSR.
In this study, all 111 subjects treated with the ExFeel implant were included, and 11 implants failed before loading, resulting in 95.3% survival rate. There were no failures of any kind for 2 years after the loading. Therefore, all the failures can be attributed to lack of initial stability.
As to the composition of subjects, male subjects were 20% more than females in number. Implants and patients were evenly distributed among patients in their 20s and under, and in the 50s, but there were more male patients and more implants placed in men among patients in their 30s, 40s, and 60s. Increasing numbers of implants and patients were observed in men in their 40s and in women in their 50s.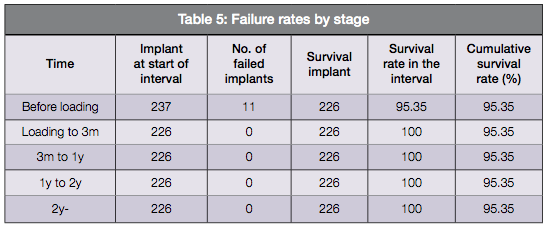
By implant location, there were 2.2 times more implants placed in the lower jaw than the upper jaw, and most in the posterior region (about 95% of all the implants) than the anterior region. A greater rate of tooth loss in the lower posterior is thought to be the reason for this, as demonstrated in the study by Meskin, Brown, et al.,1988.
There were 11 implants that did not meet the survival criteria, including one osseo-integration failure with occlusal problems, three due to smoking and drinking, one burned because of bone quality, two lost by infection, and four loosened after immediate placement or failure to osseointegrate. Among these were three cases of osseointegration failure and five cases of infection by food, drinking, or smoking. Thus the main causes of the failure include infection, drinking, smoking, and lack of osseointegration. As reported by Chuang, et al. (2001), it is thought that systemic conditions of a patient, such as diabetes, age, osteoporosis, smoking, and radiation therapy, influence implant survival rate.
Conclusion
This study was performed in a short period of time — less than 2 years — and it analyzed survival rates instead of success rates. The shortcoming of the study lies in the lack of data on prosthetic complications. Despite these constraints, the study showed a 95.35% short-term survival rate of ExFeel implants with an XPEED-treated surface, which would indicate the implant can be chosen and used as a stable option. However, a long-term study with more implants is called for.
References
1. Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1(1):11-25.
2. Bahat O. Brånemark system implants in the posterior maxilla: clinical study of 660 implants followed for 5 to 12 years. Int J Oral Maxillofac Implants. 2000;15(5):646-653.
3. Barewal RM, Oates TW, Meredith N, Cochran DL. Resonance frequency measurement of implant stability in vivo on implants with a sandblasted and acid-etched surface. Int J Oral Maxillofac Implants. 2003;18(5): 641-651.
4. Brånemark PI, Adell R, Breine U, Hansson BO, Lindström J, Ohlsson A. Intra-osseous anchorage of dental prostheses. I. Experimental studies. Scand J Plast Reconstr Surg. 1969;3(2):81-100.
5. Buser D, Mericske-Stern R, Dula K, Lang NP. Clinical experience with one-stage, non-submerged dental implants. Adv Dent Res. 1999.13:153-161.
6. Carr AB, Choi YG, Eckert SE, Desjardins RP. Retrospective cohort study of the clinical performance of 1-stage dental implants. Int J Oral Maxillofac Implants. 2003;18(3):399-405.
7. Chuang SK, Tian L, Wei LJ, Dodson TB. Kaplan-Meier analysis of dental implant survival: a strategy for estimating survival with clustered observations. J Dent Res. 2001;80(11):2016-2020.
8. Cochran DL, Buser D, ten Bruggenkate CM, Weingart D, Taylor TM, Bernard JP, Peters F, Simpson JP. The use of reduced healing times on ITI implants with a sandblasted and acid-etched (SLA) surface: early results from clinical trials on ITI SLA implants. Clin Oral Implants Res. 2002;13(2):144-153.
9. Cutler SJ, Ederer F. Maximum utilization of the life table method in analyzing survival. J Chronic Dis. 1958;8(6):699-712.
10. Finne K, Rompen E, Toljanic J. Clinical evaluation of a prospective multicenter study on 1-piece implants. part 1: marginal bone level evaluation after 1 year of follow-up. Int J Oral Maxillofac Implants. 2007;22(2):226-234.
11. Friberg B, Henningsson C, Jemt T. Rehabilitation of edentulous mandibles by means of turned Branemark System implants after one-stage surgery: a 1-year retrospective study of 152 patients. Clin Implant Dent Relat Res. 2005;7(1):1-9.
12. Hämmerle CH, Jung RE, Feloutzis A. A systematic review of the survival of implants in bone sites augmented with barrier membranes (guided bone regeneration) in partially edentulous patients. J Clin Periodontol. 2002;29 Suppl 3:226-231; discussion 232-3.
13. Lee SY, Yang DJ, Yeo S, An HW, Ryoo KH, Park KB. The cytocompatibility and osseointegration of the Ti implants with XPEED® surfaces. Clin Oral Implants Res. 2012;23(11):1283-1289.
14. Martinez H, Davarpanah M, Missika P, Celletti R, Lazzara R. Optimal implant stabilization in low density bone. Clin Oral Implants Res. 2001;12(5): 423-432.
15. Meredith N. Assessment of implant stability as a prognostic determinant. Int J Prosthodont. 1998;11(5):491-501.
16. Meskin LH, Brown LJ. Prevalence and patterns of tooth loss in the employed adult and senior populations, 1985-1986. J Dent Educ. 1988;52(12):686-691.
17. Misch CE. The implant quality scale: a clinical assessment of the health-disease continuum. Oral Health. 1998;88(7):15-20, 23-25; quiz 25-26.
18. Park JW, Kim HK, Kim YJ, An CH, Hanawa T. Enhanced osteoconductivity of micro-structured titanium implants (XiVE S CELLplus) by addition of surface calcium chemistry: a histomorphometric study in the rabbit femur. Clin Oral Implants Res. 2009;20(7):684-690.
19. Penarrocha M, Carrillo C, Boronat A, Marti E. Early loading of 642 Defcon implants: 1-year follow-up. J Oral Maxillofac Surg. 2007;65(1):2317-2320.
20. Rosenberg ES, Cho SC, Elian N, Jalbout ZN, Froum S, Evian CI. A comparison of characteristics of implant failure and survival in periodontally compromised and periodontally healthy patients: a clinical report. Int J Oral Maxillofac Implants. 2004;19(6):873-879.
21. Schnitman PA, Shulman LB. Recommendations of the consensus development conference on dental implants. J Am Dent Assoc. 1979;98(3):373-377.
22. Seong-Yeon Lee, Young-Kyun Kim. Retrospective clinical study of tapered form dental implant system. The Journal of the Korean Academy of Implant Dentistry. 2010;29(2):20-25.
23. Smith DE, Zarb GA. Criteria for success of osseointegrated endosseous implants. J Prosthet Dent. 1989;62(5):567-572.
Stay Relevant with Implant Practice US
Join our email list for CE courses and webinars, articles and mores
Read our following terms and conditions before subscribing.


