Drs. Brenda Baker and David Reaney look at the pros and cons of the two key retention methods at the heart of restoring implants
 Both cement- and screw-retained pros-theses have been validated in clinical studies, and each type of restoration has particular advantages and disadvantages. Historically, screw-retained prostheses were widely used, as restorations could be retrieved for evaluation of the underlying implants and repair of any possible complications. Cemented restorations are now widely used as more esthetic restorations can be created.
Both cement- and screw-retained pros-theses have been validated in clinical studies, and each type of restoration has particular advantages and disadvantages. Historically, screw-retained prostheses were widely used, as restorations could be retrieved for evaluation of the underlying implants and repair of any possible complications. Cemented restorations are now widely used as more esthetic restorations can be created.
While they are not as readily retrieved as a screw-retained prosthesis, cementing restorations with provisional cement allows a degree of retrievability. The cement chosen is the controlling factor in the retention attained; either temporary cement or a mixture of temporary cement and petroleum jelly (reduced strength) can be used to cement implant-supported prostheses.
 The lack of screw holes in cemented prostheses provides a design that enhances the physical strength of porcelain and acrylic resin, resulting in less fracture. The occlusal surface is devoid of screw holes, and as such, the occlusion can be developed so that it responds to axial loading. Cement-retained implant prostheses provide easier access to the posterior of the mouth, reduced costs, reduced complexity of components, reduced complexity of laboratory procedures, and reduced clinical chairside time. There is some evidence that cement-retained fixed prostheses have fewer prosthodontic complications after delivery. It is generally simpler to correct a misaligned implant with a cemented restoration.
The lack of screw holes in cemented prostheses provides a design that enhances the physical strength of porcelain and acrylic resin, resulting in less fracture. The occlusal surface is devoid of screw holes, and as such, the occlusion can be developed so that it responds to axial loading. Cement-retained implant prostheses provide easier access to the posterior of the mouth, reduced costs, reduced complexity of components, reduced complexity of laboratory procedures, and reduced clinical chairside time. There is some evidence that cement-retained fixed prostheses have fewer prosthodontic complications after delivery. It is generally simpler to correct a misaligned implant with a cemented restoration.
With screw-retained restorations, if the implant is misaligned, the screw access hole may be in a variety of locations (Jacobs and O’Connell, 2011). On a posterior tooth, the screw access hole may obliterate much of the occlusal anatomy. With a screw-retained prosthesis, once the retaining screw has been tightened, the access hole is filled with a resin material. During function, this material wears and stains, and periodically needs replacement. The screw access hole may represent 50% or more of the occlusal surface of a posterior tooth, so the correct occlusal contacts must be built into the resin restoration at the chairside.
A screw access hole on an anterior implant-supported prosthesis may mean that the alignment of the implant is such that the screw access is to be placed buccally or near the incisal edge. In that case, access holes may be filled with tooth-colored resin in the provisional restoration, but the final restoration would warrant a cement-retained prosthesis.
Whereas cement-retained prostheses are constructed using conventional prosthodontic procedures, screw retention requires extreme care because of the small retaining screw, which may be lost in or outside the mouth. Drivers used to tighten the retaining screws may be difficult to align in the posterior areas of the mouth. These retaining screws, being smaller than the abutment-to-implant screws and typically placed with lower torque (10Ncm compared to 32Ncm), are also liable to loosen, which has been well documented in many clinical studies.
A minimum of 7 mm from the implant head to the opposing tooth is advised for adequate retention of a cement-retained restoration. A screw-retained prosthesis may be provided with 4 mm of interocclusal space. Excess cement can be difficult to clear from the subgingival margin of a restoration, which can lead to persistent inflammation of the tissue. It is important that cemented restorations are designed with the prosthesis-abutment interface no more than 2-3 mm subgingivally, so that excess cement may be readily removed.
Occlusal and loading concepts related to design
The selection of screw retention or cement retention as an attachment mechanism impacts on the occlusion of the restoration. Implants ideally placed under the central fossa or stamp cusps of posterior teeth represent the best opportunity to generate axial loading. Clinical experience suggests that this goal is often not attained, and thus, offset loading occurs. Screws or screw holes in the occlusal surfaces of teeth disrupt the occlusal surfaces. The area where the screw hole exists may be a critical area when one attempts to generate an optimal occlusion.
With cement-retained implant restorations, all of the anatomic surfaces of all of the teeth are present to develop protrusive and lateral protrusive relationships. Screw-retained implant prostheses may lack the proper anatomy on the cuspids and central incisors for the smooth transition into protrusive and lateral protrusive movements, and thus, anterior guidance may be compromised.
Many factors interact in a complex manner to produce a load at the bone-implant interface. Offset loading is one factor that can be controlled with prosthetic design. The bone-implant interface appears able to survive with some degree of offset loading; however, there appears to be an increase in the incidence of prosthetic complications such as screw loosening and breakage. As such, prudent control of offset loading is suggested through prosthetic design. The ability to generate vertical or axial loading may be compromised when the choice is made to use screw-retained implant restorations. Cement-retained implant prostheses are able to vertically load the prosthetic head of the implant.
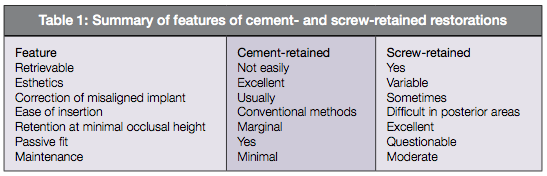
Features of cement- and screw-retained restorations
Table 1 compares some of the key features of cement- and screw-retained restorations.
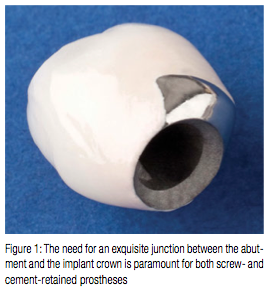
One of the keys to successful long-term implant restorations is the stability of the implant/abutment connection.
The type of finish on screws can have a significant effect on the tension induced by a given torque. Implant manufacturers have altered the material in the screws as well as the surface of abutment screws in an effort to prevent or minimize screw loosening. Martin and colleagues (2001) tested the rotational angles in implant/abutment connections with various abutment screws and preloads. They found that the abutment screws with enhanced surfaces reduced the coefficient of friction and produced greater rotational angles and preload values than screws made from conventional gold and titanium alloys.
Abutment selection
Abutments are components that attach directly to the head of the implant and extend through the gingiva and into the oral cavity. For fixed prostheses, the abutment acts as a substitute for the missing coronal tooth structure. A variety of abutments are available, which allow the restorative dentist the ability to provide a functional and esthetic restoration. Some abutments are designed to be prepared directly in the mouth (or milled in the laboratory), similar to conventional crown preparations. Other abutments are customized in the laboratory and cast to their final shape. With both of these techniques, the final restoration is cemented onto the finished abutment.
In other designs, factory-prefabricated abutments are used, and the prosthesis is screwed directly onto the abutment. Abutment selection depends on many clinical factors, and it is often not possible to make this selection until after second-stage surgery maturation of the soft tissues has occurred. In difficult situations, it is best to wait until the working cast has been made and mounted on an articulator before choosing the abutment. The abutment must take account of the position and angulation of the implant, the height and thickness of the surrounding soft tissues, the interocclusal space, and the type of restoration to be placed. Additional considerations include the height of the lip line, the occlusal scheme, and the position of the tooth in the arch.
The primary objective must always be proper support of the surrounding tissues and optimal morphology to support the restoration without impairing hygiene maintenance. These goals can be easily achieved if the abutment is custom-made, but for the purpose of complete analysis of all available options, the clinician is presented here with the spectrum of current possibilities.
Abutment types
UCLA abutment – The UCLA abutment is a very versatile abutment (Lewis, et al., 1992). It may be used to produce a customized abutment for a cemented restoration or as a screw-retained restoration. The abutment consists of a machined gold cylinder with a plastic sleeve that can be shaped to allow the construction of a custom abutment. The abutment and restorative coping are incorporated into one unit, reducing the number of interfaces and components in the restored implant pillar.
The abutment sleeve is then waxed up in the laboratory to the shape of a core that fits the particular tooth it is replacing, and can also be shaped to compensate for any misalignment of the implant. This abutment design allows for a wide range of tooth sizes and angulations to be accommodated, but with a machined-fitting surface to ensure accurate fit of the abutment on the implant.
The UCLA abutment may correct problems of implant angulation by up to 30°. This feature helps provide an esthetic restoration by creating a substructure with a good emergence profile and contours that accurately follow the gingival tissue. The finished abutment is screwed down directly onto the implant, and a coronal restoration is cemented onto the post. The UCLA abutment gives the laboratory the scope to produce an optimum abutment and save clinical time, especially in challenging cases.
The UCLA abutment comes in two designs with either a hexagonal or non-hexagonal fitting surface to engage the head of the implant. The hexagonal UCLA abutment makes for a non-rotational design that allows it to be used for single-unit restorations. The non-hexagonal version does not engage the hexagonal top of the implant and can be used for multiple-unit restorations.
The machined collar on the UCLA abutment is 1 mm high and so can be used where there is minimal soft tissue height above the implant head. In an esthetic area, however, if there is a risk of metal showing through thin gingival tissue, an alternative abutment may be required. Many dentists cement fixed-implant prostheses with temporary luting cement, so the restoration may be removed at some later date. This would be important if the abutment screw were to break or get loose. Then a new screw could be placed without having to remake the prosthesis.
Despite the flexibility of the UCLA abutment, the overall cost of the restoration can be high. The abutment must be purchased, and there is a laboratory charge for waxing and casting the abutment. The final restoration must then be fabricated on the finished abutment. The UCLA can also be made to make a screw-retained prosthesis. The abutment is waxed up to the full contour of the final restoration and may be cut back for porcelain if required. Hence, the abutment and restoration are in one piece, and they are retained by an abutment screw. With this type of restoration, the positioning of the implant is critical since the screw access hole should pass through the cingulum area of an anterior tooth or the central fossa of a posterior tooth. Poor placement of the implant may lead to abnormally shaped cingulum areas or access holes that affect the occlusal morphology of posterior teeth, leading to a poor occlusal relationship.
Preparable abutments – A range of implant abutments is available that can be prepared with cutting burs to the desired shape. A cement-retained prosthesis may then be made over the prepared abutments. Preparable abutments may be used for single crown or multiple units. Preparable abutments are most effective where the implant placement is favorable, and so there is minimal preparation to be completed on the abutment. The preparation of the abutment may be completed intraorally by the dentist or in the laboratory by the technician. Direct preparation of the abutment in the mouth is completed using the same principles as tooth preparation. A silicone matrix of the fully contoured wax-up is useful as a guide to abutment preparation. Preparable abutments are available with different collar heights to suit the thickness of soft tissue present above the implants. The abutments may be made of metal (usually pure titanium) or ceramic, which is used in critically esthetic areas.
Titanium abutments – Titanium abutments may be covered with a gold-colored titanium nitride coating that improves esthetics (Sadeq, et al., 2003). The gold color is less likely than a titanium-colored abutment to cast a gray shadow at the gingival margin. The abutment is normally machined with a 6° taper and has a pre-chamfered margin. It is available straight or pre-angled to correct for misalignment of the implant. The abutment has a flat side to prevent rotation of the final restoration.
Ceramic abutments – Ceramic abutments may be made of zirconia or alumina (aluminium oxide) (Lesmes and Lasterl, 2011). The ceramic allows for light reflection in a similar way to natural teeth and leads to less darkening of thin gingival tissue than is the case with metal. The ceramic abutment may be preferred if a translucent material is used for the definitive prosthesis (Christensen, 2008).
The zirconia abutment has a machined titanium interface that fits onto the implant. The margins of the abutment can be prepared to follow the uneven contours of the gingival tissue.
The hardness of the material can make these abutments difficult to prepare intraorally. The implant position should be as close to ideal as the abutment cannot accommodate changes in angulation.
Prefabricated conical abutments: screw-retained prostheses
The conical abutment is one of several pre-machined abutments that are used for screw-retained restorations. It has a side wall taper of 15° with hexagonal sides to resist rotation of the restoration, where needed. Other tapered abutments are angulated from 25° to 35° to correct for the difference in orientation between implant and restoration.
While the use of misaligned implants is sometimes unavoidable, it should be minimized as non-axial forces on implants and abutments are more likely to cause complications and failures. If possible, the clinician should avoid lateral excursions on teeth that have angulated abutments. Angled abutments facilitate restoration of implants placed with buccolingual or mesiodistal misalignment (Cavallaro and Greenstein, 2011). A 15° angulation of a prefabricated abutment can create parallelism between adjacent abutments. Additionally, correcting an implant trajectory with a 15° angled abutment can shift a restoration about 1.0-1.5 mm at the occlusal aspect, and a 25° abutment can move it 2.0-2.5 mm. When using angled abutments to achieve a good prosthetic result, the clinician should leave sufficient running room to ensure a gradual emergence profile of the restoration. Running room is the vertical distance from the implant’s prosthetic platform to the free gingival margin. The clinician uses this distance to make the transition from the smaller diameter, circular shape of the implant’s coronal aspect to the larger cross-sectional shape of the tooth being restored. In the esthetic zone, it is imperative that correction of angulation issues be combined with sufficient running room (sufficiently deep placement of the implant).
Prefabricated abutments are made with a range of collar heights to accommodate the subgingival position of the implant. Selection of the collar height will allow the margin of the restoration to be placed just below the gingival margin so the emergence profile of the final restoration can be improved. However, the abutment collar is uniform in height and does not follow the natural contours of the tissue. The screw-retained prosthesis requires a minimum of 4 mm of interocclusal space from the implant to the occlusal or incisal edge of the final restoration. Angulated abutments require more interocclusal space.
Machined abutments:
cement-retained prostheses
Different machined abutments are available for use with cemented prostheses.
These abutments are designed for minimal modification and so can be used only where implant placement is ideal, and there is ample space for the prosthesis. A parallel-sided hexagonal abutment can be used for single restorations — the crown can be fabricated directly onto a gold or ceramic coping that is machined to fit onto the abutment. Tapered abutments are generally used for multi-unit prostheses and may be straight or angulated. Prefabricated abutments
are not commonly used due to their lack
of flexibility.
Standard abutment – The original abutment for the external hex implant was the standard abutment. This two-piece abutment consists of a cylinder and a screw. Its purpose was to provide a restorative platform above the soft tissue level. The standard abutment requires a minimum of 2 mm of tissue height and is available up to 7 mm high.
Standard abutments now have few indications. They may be used for the fabrication of full-arch, fixed hybrid prostheses. For this purpose, a secondary cylinder, which is screwed onto the standard abutment, is incorporated into the prosthesis framework. The standard abutment may also act as the platform for some overdenture attachments.
One disadvantage of the standard abutment is that the collar has a uniform height and so does not follow the natural contours of the gingival margin. It is thus difficult to achieve an appropriate emergence profile and acceptable esthetics. As with other intermediate-type abutments, it requires the cost and complexity of a second restorative component and screw.
Custom-machined abutments – The trend toward impressing the implant and reproducing it in the laboratory, rather than using a registration of a prefabricated, stock abutment placed on top of the implant, has hugely increased the flexibility of implant prosthodontics and created a new standard for esthetic implant restorative dentistry.
Advances in CAD/CAM have made it possible to manufacture precision custom abutments. Once an impression of the implants is obtained, the CAD/CAM system allows for the design of individual abutments by computer or the scanning of an abutment wax-up. The specifications are then transmitted to a centralized facility, and a metal or ceramic abutment is machined and then returned to the local laboratory.
The advantage of this approach is that the abutment can take into account implant angulation, tissue height, and the size and contour of the final restoration. As it is a one-step process, the custom-machined abutment eliminates the need to buy a stock abutment and then modify it in the laboratory. The centralization of the manufacturing process means that the abutments can be produced with an accurate fit.
Greater angulation correction issues of more than 15° are well controlled by the custom-made components. Another option is to construct a final custom abutment based on the use of a special two-piece healing abutment (Drago, 2007). The healing abutment has codes embedded on its occlusal surface containing the information needed to create the final abutment.
It provides the position of the implant hex, the soft tissue height, and the implant platform diameter.
A simple conventional elastomeric impression is made of the healing abutment, thus ensuring reproduction of the coded area. The master cast is scanned in a CAD/CAM laboratory where an abutment is designed and milled. A crown can then be made and sent to the dentist for issue.
This system eliminates the need for implant-level impressions and simplifies the restorative technique.
Conclusion
The current aim of implant design is to address situations prone to failure such as cases of low bone quality or of concomitant systemic disease. There are more than 1,300 dental implant types available worldwide, each with differing properties (size, shape, and surface). Emerging developments are based mainly on modification of either chemical or mechanical properties of an implant.
With the expansion of routine implant restoration, from the edentulous arch to the partially edentulous arch and to single-tooth replacement, a broader array of restorative abutments and components have been necessary, compared to implant treatments limited to the edentulous mandible. Accordingly, implant manufacturers have expanded abutment choices substantially.
The practice of implant-level impression taking can be traced directly to the UCLA abutment concept, from which a number of abutment options have evolved.
The trend toward impressing the implant and reproducing it in the laboratory, rather than using a registration of a prefabricated stock abutment on top of the implant, has greatly increased the flexibility of implant prosthodontics and created a new standard for esthetic implant restoration.
References
- Christensen GJ. Selecting the best abutment for a single implant. J Am Dent Assoc. 2008;139(4):484-487.
- Cavallaro J Jr, Greenstein G. Angled implant abutments: a practical application of available knowledge. J Am Dent Assoc. 2011;142(2):150-158.
- Drago C. Implant Restorations: A Step-By-Step Guide. 2nd ed. London: Wiley-Blackwell; 2007.
- Jacobs SH, O’Connell BC. Dental Implant Restoration: Principles and Procedures. Berlin: Quintessence; 2011.
- Lesmes D, Laster Z. Innovations in dental implant design for current therapy. Dent Clin North Am. 2011;55(4):649-661.
- Lewis SG, Llamas D, Avera S. The UCLA abutment: a four-year review. J Prosthet Dent. 1992;67(4):509-515.
- Martin WC, Woody RD, Miller BH, Miller AW. Implant abutment screw rotations and preloads for four different screw materials and surfaces. J Prosthet Dent. 2001;86(1):24-32.
- Sadeq A, Cai Z, Woody RD, Miller AW. Effects of interfacial variables on ceramic adherence to cast and machined commercially pure titanium. J Prosthet Dent. 2003;90(1):10-17.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores


